During 2018 The Christie will be the first NHS site to treat patients with high-energy proton beam therapy (PBT). Our research is central to this clinical provision and will ensure that patients always have access to the latest developments in the field.
Proton beam therapy (PBT) is a radically new type of radiotherapy. It has the potential to improve the precision and targeting of radiation therapy (RT) leading to fewer side effects, faster recovery and better outcomes for patients. It also has the potential to target radio-resistant hypoxic tumours and other tumours that are difficult to treat by more conventional means.
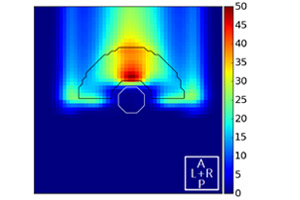
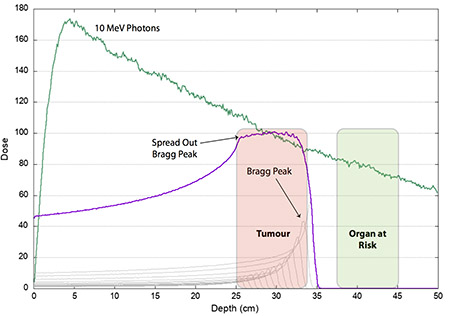
In PBT, unlike conventional X-ray radiotherapy, protons deliver the dose in a Bragg peak. By modulating the energy and position of the Bragg peak the dose can be painted over the tumour volume allowing more dose to be delivered to the tumour while sparing the healthy tissue surrounding it. PBT also offers the potential to treat tumours, very close to critical organs, because there is no exit dose.
Further useful information is provided within the Benefits of proton beam therapy at The Christie video (The Christie, 6.19: YouTube).
Scientific and technological challenges of PBT
PBT is still in its infancy and there are a number of scientific and technological challenges that need to be addressed for it to achieve its full potential.
Our current major research activities are aimed at tackling the key scientific and technological challenges for PBT:
- biological optimisation
- range verification
- proton imaging
- computational oncology
- new accelerator developments for PBT
- translational technical radiotherapy
- translational radiobiology
- clinical trials

The PRECISE group
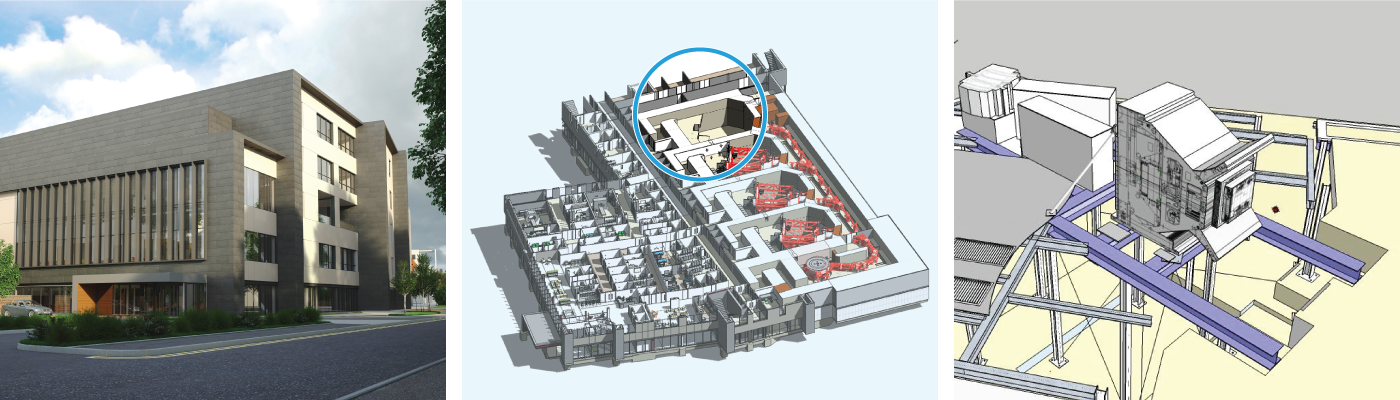
Our PBT research is undertaken by the PRECISE group (Proton research at The Christie and the University’s Division of Cancer Sciences). The group has a dedicated research facility – known as the ‘research room’ within the clinical proton therapy centre aimed at addressing these challenges.
The research in PRECISE takes a multidisciplinary approach spanning from basic research to applied and translational research leading in to clinical trials. The research is designed to improve the outcomes for patients both in terms of survival and quality of life.
The multidisciplinary research team brings together The University of Manchester, The Christie and the Manchester CRUK Major Centre. The group has seen rapid growth and now has over 30 researchers with academic and clinical expertise.
The PRECISE group is led by Professor Karen Kirkby.
Funding
The PRECISE group currently has secured funding of around £15m. This comes from most major research funding bodies in the UK including CRUK, EPSRC, STFC and NC3Rs, and EU Horizon 2020. We are also part of the NIHR Manchester Biomedical Research Centre and the Manchester CRUK Major Centre.
Research room
The research room is located within the Christie Clinical Proton Beam Centre. It has been developed in parallel with the clinical treatment facility and is a unique research resource. It will be available to national and EU users through the EPSRC Network grant and EU grant INSPIRE.
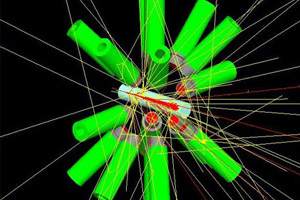
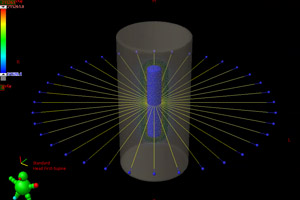
The room features a pencil beam scanning nozzle which is the same as that used in the clinical facilities. This ensures our experiments can emulate the beam delivery in the gantry treatment rooms in the clinical centre.
The research room has two horizontal beam lines which transport the beam to the scanning nozzle and then to modular experimental end-stations. These end-stations are interchangeable to allow the maximum flexibility in the design of experiments and optimum use of the beam time available for research.
Adjoining the research room there is a biological preparation room for setting up experiments. It will have tissue culture facilities and access to hypoxia cabinets. There is also a control room for remotely controlling the beam and experimental end-stations.
Watch How proton beam therapy will be delivered at The Christie (The Christie, 1:52: YouTube) for further information.
A national and European facility
It is envisaged that the research room will be run as a national facility. This will allow external researchers to undertake their high-energy proton experiments here.
Please contact us for more information, including how to access the facility.
Major research activities
Our research aims to address all the main challenges of PBT. Activity is currently focused on a number of key areas spanning the full scale of PBT research, from utilising computational simulations through to experiments in our research room.
Biological optimisation
Biological optimisation includes how protons are different to photons; relative biological effectiveness; biologically optimised treatment planning; and mapping the PBT dose to the tumour and its microenvironment).
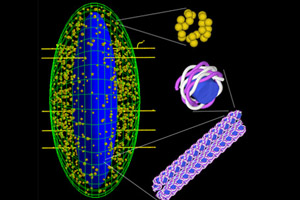
Monte-Carlo modelling of proton induced DNA damage and repair
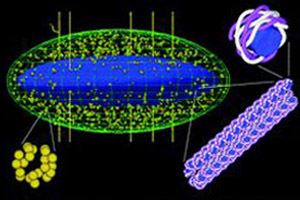
We use radiation track structure simulation to model the interaction of protons with DNA to predict the complexity and quantity of damage across the proton Bragg peak. We have developed mechanistic in silico models for DNA repair to investigate the biological response of the cells to proton induced DNA damage.
Lead researcher: Michael Merchant
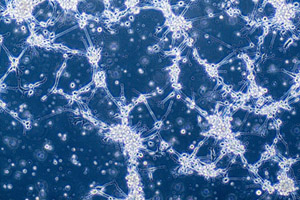
Biology and hypoxia
We are exploring the biological response to PBT in a variety of tumour types. This work includes investigating the relative biological effectiveness of proton beam therapy, the DNA damage responses and influence of the tumour microenvironment. We are also developing biologically-relevant dosimetry tools.
Lead researcher: Amy Chadwick
Range verification
Range verification using prompt gamma
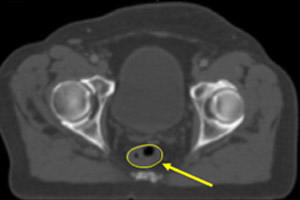
This project aims to reduce the consequences of undetected patient anatomical changes during PBT. Through the detection of the high-energy gamma-rays emitted during PBT, anatomical changes can be determined. The planned dose distribution can then be modified, thereby adapting the therapy to deliver a more personalised course of treatment.
Lead researcher: Michael Taylor
Computational oncology
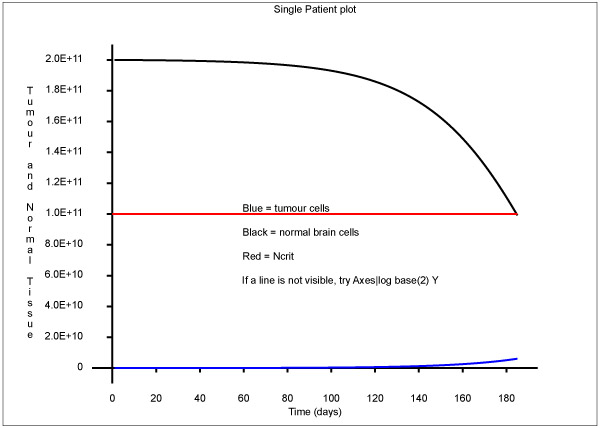
Cell cycle and top-down modelling
Radiation sensitivity is known to vary around the cell cycle and we are interested in exploiting changes in age distribution during RT. Similarly, working from the 'top down' we have developed models of patients, their response to RT, and the resulting changes in their survival, and are using these models to estimate biological parameters of the population from fitting to clinical trial data.
Lead researcher: Norman Kirkby

National treatment demand simulation and data
The Malthus Project uses evidence-based clinical decisions and maps them in a discrete-event simulation. It combines this with granular Public Health England cancer datasets and population data to map cancer treatment demand across the country.
Lead researchers: Norman Kirkby and Thomas Mee
New accelerator developments
Investigating the clinical benefit of new accelerator developments for proton therapy
In this joint project with the Department of Physics and Astronomy and the Christie Medical Physics and Engineering we investigate the properties of proton therapy accelerators that are required to deliver a clinical benefit to proton therapy. A specific focus of this project is proton arc therapy.
Lead researchers: Michael Merchant and Rob Appleby
Proton imaging

Proton CT
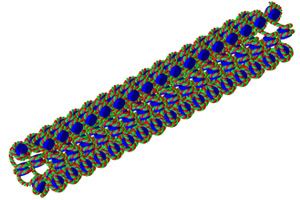
We are working as part of a national programme led by Professor Nigel Allinson (University of Lincoln) on the development of proton CT.
Lead researchers: Karen Kirkby and Ranald Mackay
Translational technical radiotherapy

Advanced radiotherapy
PRECISE works with clinical radiotherapy at The Christie to improve the delivery of proton therapy. This is achieved by integrating clinical physicists as part of the PRECISE team working across a number of the research projects. Particular interests are improvement in proton treatment planning and verification.
Lead researchers: Ranald Mackay and Adam Aitkenhead
Clinical trials
Proton Beam Therapy (PBT) is an important treatment modality in modern radiotherapy, but its exact role and value have yet to be fully established. The University of Manchester and The Christie will lead the clinical evaluation of PBT, and will integrate fundamental research on PBT into patient-centred trial development.
Lead researcher: Neil Burnet
Networks and training
Training
We run two educational training programmes:
Networks
We host two UK networks:
- Global Challenge Network+ in Advanced Radiotherapy
Bringing clinical and Science and Technology Facilities Council (STFC) communities together - the STFC community includes particle physics, astronomy, detector and large computing. - EPSRC proton therapy network
Bringing the engineering and science community together with the clinical community, and creating a national infrastructure for PBT.

Contact us
- Back to Cancer